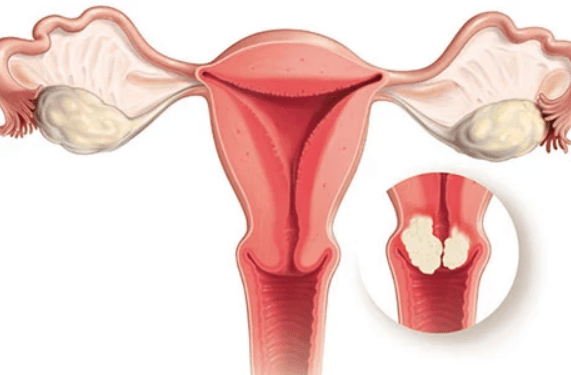
Currently cervical cancer ranks the second position among all malignant neoplasms in women. The incidence rate, despite significant progress in diagnostic, treatment and prevention of this pathology, remains high and is 20 women per 100,000. The mortality rate, unfortunately, also remains high, mainly due to the late diagnosis of the disease. And although the peak incidence occurs at the age of 35-45, this ailment is getting "younger" and now increasingly affects women under 30.
Cervical cancer, like most cancers, is asymptomatic for some time. The period from the "genesis" of a tumor to clinical manifestations in the later stages is on average 7-15 years. Agree, there is plenty of time to detect the disease at an early stage and get rid of it completely. But in order to do this, women must regularly visit a gynecologist and undergo preventive examinations on time.
Importantly! Thanks to the modern diagnostic strategy – cervical screening (cytological examination of material from cervical canal of cervix), it is possible to clearly recognize even the stage of precancerous changes. And if the disease is detected in the early stages, treatment effectiveness is 100%.
Why should cervical cancer be diagnosed as early as possible? Early metastasis is a feature of malignant tumors of this localization. Even at stage 1, the neoplasm can metastasize.
Risk factors for cervical cancer development
Despite of risk factors of cervical cancer development in woman does not mean that she will necessarily get the disease, but they significantly increase the basic risk of developing this pathology.
The main risk factor for cervical cancer development is long-term persistence of HPV (human papillomavirus) infection. HPV is a very common sexually transmitted infection. Most sexually active people have it, were or will be in the future. Unfortunately, most women and men do not even know that they are infected, since HPV does not manifest itself clinically.
In most people, the immune system rids the body of HPV over time, that is, the virus disappears, but it can cause damage during its stay in body. Changes in epithelial cells of cervix before turning into a tumor last for years. Unfortunately, it is currently unknown why some women with persistent HPV develop cervical cancer while others do not.
To date, more than 100 types of human papillomaviruses are known, all of them are grouped by the ability to cause oncological pathology into HPV of high, medium and low oncogenic risk. The most dangerous types of HPV include 16 and 18.
Other known risk factors:
- smoking;
- use of oral contraceptives;
- the beginning of sexual life at an early age;
- a large number of sexual partners;
- unprotected sexual contact with barrier methods of contraception;
- certain autoimmune and immunodeficiency diseases;
- sexually transmitted infections;
- unhealthy diet and low physical activity.
Obviously, we can influence on most of listed risk factors and avoid the behaviors that can generate them, which is nothing more than primary prevention of cervical cancer.
Cervical cancer vaccination: myth or reality?
We have already understood that one of the most significant risk factors for cervical cancer development is HPV infection, therefore vaccination against the human papillomavirus protects against cervical cancer. Therefore, vaccination against this malignant disease really exists.
Vaccination of girls and boys aged 9-14 is the most effective, as they are less likely to encounter HPV. But adults up to 45 years old are also vaccinated.
Importantly! The vaccine prevents infection with certain types of HPV (against which it is developed), but not all. Also, the vaccine does not treat pre-existing HPV infection, cervical dysplasia, or cervical cancer.
Currently, 2 HPV vaccines are available in Ukraine:
- Cervarix, which protects against 16 and 18 types of virus;
- Gardasil-4, which protects against 6, 11, 16 and 18 types of the virus.
There is also a Gardasil-9 vaccine that protects simultaneously against 9 types of HPV, but it is currently unavailable to Ukrainians.
Early diagnostic strategy
In 2020, the World Health Organization published a strategy according to which by 2050, the incidence of cervical cancer can be reduced by 40% in the world, which will prevent 5 million deaths related to the disease.
The WHO global strategy for cervical cancer elimination outlines three main steps: vaccination for primary prevention, screening for early diagnosis and modern treatment.
Screening allows you to get information about the state of cervix, detect possible precancerous changes (for example, dysplasia) or cancer at an early stage. The basis of screening is the Pap test (cytological examination of material from cervix) and PCR to detect the DNA of virus. Every woman should visit her gynecologist regularly and undergo these screening tests.
Importantly! Today in Ukraine, doctors advise to do a Pap test for the first time from the beginning of sexual life at any age, and therefore - once a year during an annual preventive visit to a gynecologist until the age of 65, provided that the last 3 tests have not had any abnormalities.
Today, the modern Pap test based on liquid cytology, rather than the classic smear on a glass, is increasingly being used. It significantly increases the diagnostic sensitivity of cervical screening program and is FDA approved for mass use. Therefore, if the doctor offers to a patient a choice, liquid cytology should always be chosen, not the classic smear.
Complement screening with testing for HPV presence. Detection of the pathogen's DNA using the polymerase chain reaction method also makes it possible to determine its type and classify it according to the degree of oncogenic risk. It is important to understand that HPV is not detected in order to treat. Unfortunately, no specific treatment methods for viral papilloma have been developed to date. This is necessary in order to choose the right strategy for the follow-up of a woman, because she automatically falls into the risk group of cervical cancer developing and needs more careful and frequent monitoring.
Possibilities of cervical cancer treatment
A whole multidisciplinary team consisting of an oncologist, a chemotherapist, and a radiologist can be involved in treatment program of cervical cancer. There is no single treatment scheme for cervical cancer. So often patients are offered a choice of several therapy methods and their combination. First of all, the treatment strategy is related to the stage at which the malignant neoplasm is diagnosed.
Surgical treatment is the main method of cervicalcancer treating. The extent of surgical intervention is determined by the stage of the disease. It can be both an organ-preserving surgery (conization of cervix, wedge-shaped resection) and a complete removal of cervix, sometimes together with uterus and appendages, regional lymph nodes, and omentum. Today, in modern clinics, all these interventions are performed through a minimally invasive laparoscopic approach, that is, without large incisions in anterior abdominal wall.
Radiation therapy often complements surgical treatment. Radiation therapy can be remote (with the help of special devices for treatment – linear accelerators) and contact (brachytherapy) – when the radioactive material in special applicators is brought directly to the tumor, due to which the surrounding healthy tissues are exposed to less radiation.
Systemic therapy can also be prescribed in complex treatment:
- chemotherapy, according to modern world treatment protocols;
- targeted therapy and immunotherapy – modern effective drugs of biological action;
- participation in clinical research.
The treatment program is made up individually for each woman, taking into account her main diagnosis, the stage of the process, existing complications, the patient's age, her general state of health, and reproductive plans.
Fertility preservation strategy
If a woman plans to become pregnant in future, then at preparation stage for treatment, she should discuss with her doctor all the possibilities of preserving fertility and together choose the most optimal one.
As a rule, natural pregnancy is possible when the disease is diagnosed at an early stage, the extent of surgical intervention was small, and the uterus and ovaries are preserved. In other cases, freezing of eggs, embryos, and surrogate motherhood are possible.
Maimonides Medical Center specialists will help you with any question related to prevention, diagnosis or modern treatment of cervical cancer. Excellent theoretical training and unique practical experience of our doctors, modern material and technical base allow us to provide qualified assistance to women, according to world standards. If you want to know more detailed information, contact us at the phone numbers and contacts indicated on the site.